‘I never thought I’d live to see my granddaughter born, now she’s 3,” says woman given year to live in 2014


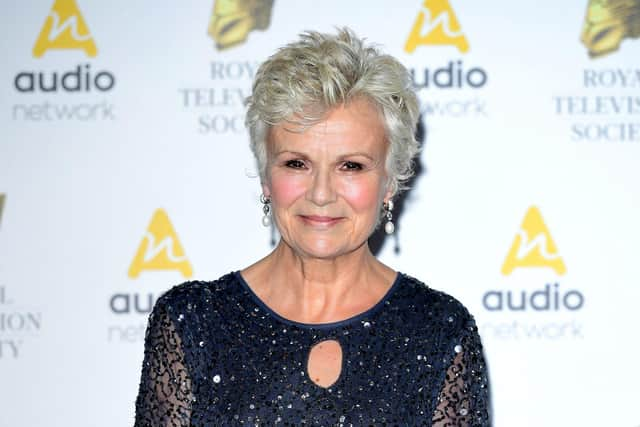
Dame Julie had visited her doctor with stomach pain, heartburn and vomiting. She was shocked when she found out she had cancer.
“These were some of the same symptoms that I’d had back in 2014,” Barbara explains. “They’re not the most common symptoms of bowel cancer like unexplained weight loss. Looking back there were signs that I ignored and put down to getting older, being overweight or drinking too much. I didn’t want to be one of the ‘worried well’ clogging up the surgery.”
Advertisement
Hide AdAdvertisement
Hide AdAlthough her cancer was discovered at a late stage and had already spread to her liver, she was able to have chemotherapy and surgery. The treatment was successful. For a while, Barbara was ‘cancer free’, and life went back to normal. But then in September 2016 – two years after her initial diagnosis – Barbara, from Harrogate, found out the cancer had returned, and this time it had spread beyond her liver to her peritoneum, a thin layer of tissue that lines the abdomen.
Barbara was told she’d have six months to a year to live if the cancer didn’t respond to treatment, and perhaps two years if it did respond.
She began a second course of chemotherapy and to her surprise it started working. Her tumours started to shrink and she began to feel more hopeful.
“When I was told I was having palliative treatment I thought that was the end. My husband and I had our wills re-written, and I took a lump sum from my pension. I tried to get as much sorted out as possible so it would be easier for my family. My oncologist didn’t expect me to respond to the chemo. When it started working, I think I headed into a bit of denial. I felt so well.”
Advertisement
Hide AdAdvertisement
Hide AdThe chemotherapy continued to work for more than two years. Barbara’s treatment became less frequent, allowing her to spend more time working and with her family.

During this time, she became involved in providing a patient perspective for bowel cancer research. She joined the UK Colorectal Cancer Intelligence Hub’s Patient-Public Group, which provides support to Yorkshire Cancer Research’s Bowel Cancer Improvement Programme.
“I became interested in helping researchers understand how things affect patients. It didn’t matter if it was too late for me or not relevant to me directly. It became a way of paying something back for the treatment and care I’d received.
“Before my experience with cancer, I thought everyone got the same treatment across the country – then I found out they don’t even get the same treatment across Yorkshire. I wanted to contribute towards the ‘levelling up’ agenda to reduce inequalities and ensure everyone receives gold-standard treatment.”
Advertisement
Hide AdAdvertisement
Hide AdBy February 2019, Barbara’s chemotherapy was no longer keeping her cancer at bay. She was quickly put on a ‘second-line’ option, but that only worked for two rounds.


“The chemo lasted much longer than anyone expected. When it stopped working, I asked my oncologist about clinical trials and he said he’d like to put me on one, but he didn’t know of any suitable ones at that point. That’s when I decided to revisit all the research I’d done before to try to find something that might work.”
While searching online, Barbara came across a new clinical trial for a treatment called Pressurised IntraPeritoneal Aerosolised Chemotherapy (PIPAC), which is a type of chemotherapy given directly into a patient’s abdomen.
“The trial had been put up on the website that afternoon. I emailed the surgeon leading the study – Jamie Murphy at Imperial College, London – and he told me to get a referral from my consultant, which I did. I saw him for the first time in March, and that’s when he told me he thought he could operate instead.” Mr Murphy was confident he could give her the life-extending surgery she needed.
Advertisement
Hide AdAdvertisement
Hide Ad“It’s a huge operation, and there were lots of pros and cons to consider. However, I really didn’t have a choice,” Barbara explains.


The surgery took place in June and lasted more than 12 hours. After just a month, she had recovered to the point where she was able to travel to Sheffield Hallam University to teach for half a day. She visited the Lake District in August, and by September she’d completed a five-mile charity walk with her surgical team. She also completed a solo trip to Australia in November to visit a friend.
“I was told to expect to feel 70 per cent of normal after three months, and I was determined to beat that,” Barbara said. “By September, I felt fine. Taking part in an exercise programme specifically aimed at people with cancer made a huge difference to my recovery.”
Sadly a recent scan revealed a new 4cm tumour on her liver. She has been urgently referred to St James’s University Hospital, Leeds, but a decision about whether to carry out surgery to remove the tumour has been postponed for four to six weeks due to the coronoavirus outbreak
Advertisement
Hide AdAdvertisement
Hide Ad“Coronavirus was the final decider, as it would be too great a risk along with major surgery. So, I’m back in a waiting situation
“Things are very uncertain,” says Barbara. “I’m worried that surgery that isn’t lifesaving might be put on hold due to the pandemic, but there was a point when I didn’t think I’d see my granddaughter born, and now she’s three.”
Comment Guidelines
National World encourages reader discussion on our stories. User feedback, insights and back-and-forth exchanges add a rich layer of context to reporting. Please review our Community Guidelines before commenting.